Every ear in every child is different. Rob Nash discusses the rationale behind reconstructive ear surgery in children and his philosophy on timing and techniques of reconstruction.
It is rare for middle ear pathologies to be life threatening. Indeed, it is uncommon for cholesteatoma to cause facial nerve weakness, dizziness or sensorineural hearing loss. Therefore, the most common rationale for operating on the middle ear is twofold. Firstly, to prevent recurrent infection and otorrhoea, and secondly to improve or prevent worsening of hearing.
It is important to remember that whilst you can take away a residual pearl of cholesteatoma, you cannot give a child the conversations they missed, or friends they did not make, because they had a unilateral hearing loss and a smelly, discharging ear. There are a number of studies that have demonstrated a unilateral hearing loss in childhood causes impaired sound localisation, discrimination of speech in noise and potentially speech development and cognition [1]. The only way we can address this, and improve the hearing of children with chronic otitis media, is effective middle ear reconstruction. Figure 1 demonstrates a consequence of inadequate middle ear reconstruction.
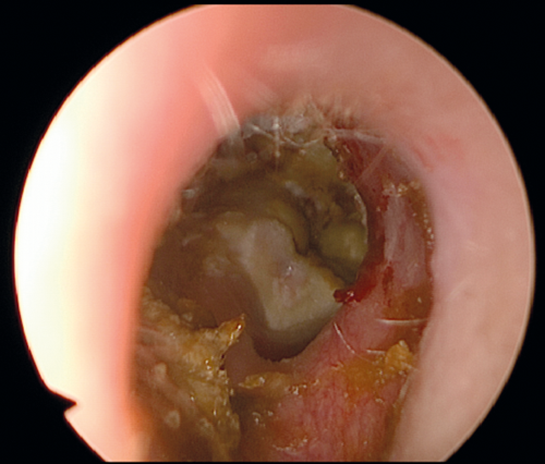
Figure 1. The right ear of a patient who has undergone canal wall down mastoidectomy,
and has ongoing infections due to tympanic membrane perforation and residual cholesteatoma.
There are a number of elements that comprise the middle ear, and many techniques described for reconstruction. The decision of which parts of the middle ear to reconstruct, when they should be reconstructed and what technique should be used depends on the extent of the original pathology, the characteristics of the patient, and the experience of the surgeon.
The most commonly reconstructed part of the middle ear is the tympanic membrane. This may be in the form of myringoplasty for perforation, or as part of a complex cholesteatoma surgery. Due to the prevalence of this operation, a number of techniques have been described, and surgeons consequently have a number of decisions to make. How should the ear be approached? Should an external incision be used? Should an endoscope be used? Should a tympanomeatal flap be raised? What grafting material should be used?
“Whilst you can take away a residual pearl of cholesteatoma, you cannot give a child the conversations they missed, or friends they did not make.”
Should the grafting material be placed in one piece, or a number of different pieces? How should the grafting material be secured in place? Broadly speaking, there is no single correct answer to any of these questions. However, the evidence suggests that cartilage may have slightly higher success rates of perforation closure. Clearly, the surgeon should use a technique with which they are familiar, and they should audit their results to ensure their outcomes are satisfactory.
In children, the most difficult decision to make when considering tympanoplasty is whether or not to operate. It is recognised that a proportion of perforations may heal spontaneously over a period of time [2]. The decision of how long to leave a perforation depends on the likelihood of spontaneous closure, and a discussion with the child and their family about how bearable the symptoms are. A recent meta-analysis suggested that age should not be a factor in these decisions, as success rates are not dependent on age, as was previously thought [3].

Figure 2. Focal retraction of the postero-superior segment of a left
tympanic membrane with a suspicion of early ossicular erosion.
Even more challenging is the decision on when to perform tympanoplasty for retraction of the tympanic membrane in cases like those shown in Figure 2. There is no satisfactory evidence to guide surgeons in these situations. The state of the contralateral ear is important. The role of grommets is unclear, but this may be a low morbidity option. It is clear that a proportion of patients with retraction will have erosion of the ossicular chain, and even develop cholesteatoma. It is also clear that reinforcement tympanoplasty may be unsuccessful, and complicated by poor postoperative hearing, or even implantation cholesteatoma. Tympanoplasty for focal, earlier retractions is technically much easier, and therefore has better outcomes, than surgery for more extensive, established retraction.
In those patients in whom cholesteatoma or retraction has eroded the ossicles, reconstruction of the ossicular chain brings further considerations. Endogenous materials such as incus interposition, exogenous prostheses, or bone cement? Partial or total reconstruction? Reconstruction onto the stapes or oval window? Concomitant malleus replacement? Tension – tight prostheses may be more stable, but give worse hearing outcomes? In total replacement, the support of the prosthesis in the oval window also needs to be considered. Total replacement tends to have worse outcomes than partial replacement. Once again, a combination of the pathology, patient, and surgeon will determine the answers to these questions [4].
“Tympanoplasty for focal, earlier retractions is technically much easier, and therefore has better outcomes than, surgery for more extensive, established retraction.”
Our last consideration is reconstruction of the canal wall. There will be cases when the canal wall will be eroded by disease, or removed by the surgeon to achieve disease clearance. The canal wall is primarily reconstructed to prevent infection and recurrence, although hearing outcomes may well also be superior in this patient group than those with an open cavity. There is increasing evidence to support the practice of ‘front to back’ tympanomastoidectomy with concomitant mastoid obliteration. In the Netherlands, the ‘bony obliteration tympanoplasty’ has been popularised [5]. Whilst canal wall reconstruction can be taken to refer to the entire posterior canal wall, it can also refer to reconstruction of the attic, which is commonly done with cartilage grafts.
“There is increasing evidence to support the practice of ‘front to back’ tympanomastoidectomy with concomitant mastoid obliteration.”
In summary, we have a lot to offer these patients. There are cases where decision-making may be challenging, but it is important to consider the rationale of ear surgery. We operate on children’s ears for the sake of their hearing and to prevent infection, and to do this, we need to reconstruct the middle ear. Reconstruction should therefore be a central consideration in every ear operation.
References
1. Lieu JE, Tye-Murray N, Karzon RK, Piccirillo JF. Unilateral hearing loss is associated with worse speech-language scores in children. Pediatrics 2010;125(6):e1348-55.
2. Rollin M, Rogers P, Robinson P. Natural history of pediatric tympanic membrane perforation. Otol Neurotol 2011;32(2):246-51.
3. Hardman J, Muzaffar J, Nankivell P, Coulson C. Tympanoplasty for Chronic Tympanic Membrane Perforation in Children: Systematic Review and Meta-analysis. Otol Neurotol 2015;36(5):796-804.
4. Bance M. Optimizing Ossicular Prosthesis Design and Placement. Adv Otorhinolaryngol 2018;81:14-23.
5. van Dinther JJS, Coopman R, Vercruysse JP, et al. The Bony Obliteration Tympanoplasty in Pediatric Cholesteatoma: Long-term Hearing Results. Otol Neurotol 2018;39(6):715-23.




