Some adults struggle with hearing in noise despite normal audiograms. Tools like the HHIA, low-gain devices and auditory training can help identify and support these cases. In this article, Angela Alexander and Fatima Abbas use a case study to discuss their approach to APD management.
Some adults who report hearing difficulties show normal results on standard audiograms. This suggests that their issues may not be related to the ability to detect sound but instead of how their brains process auditory information.
This type of difficulty often falls under the definition of auditory processing disorder (APD). To identify these individuals and effectively support them, audiologists can use tools like the Hearing Handicap Inventory for Adults (HHIA) [1]. This article presents the case of a client named Jackie to illustrate how the HHIA can help detect APD red flags, track treatment progress, and validate outcomes from auditory training and low-gain hearing devices.
Understanding the Hearing Handicap Inventory for Adults
The HHIA is a 25-item questionnaire designed to assess how hearing difficulties affect a person’s everyday life. Each question has three possible answers – yes, sometimes or no – scored as 4, 2 and 0, respectively. One such question is: ‘Does a hearing problem cause you to feel depressed?’ Higher scores indicate a more significant impact on a person’s life due to hearing difficulties [1]. The HHIA is particularly valuable for identifying APD in patients who show normal results on conventional hearing tests.
Case study: Jackie’s journey with APD
Jackie, a patient at Dr Angela Alexander’s clinic, is an example of how the HHIA can be used to identify and monitor APD. Despite normal hearing thresholds, Jackie had long experienced challenges in understanding speech in noisy environments, retaining information and following conversations. Her family dismissed her difficulties as inattention, but these experiences led to frustration and social isolation. Jackie’s situation is not unique; many adults with normal audiograms and high HHIA scores exhibit similar symptoms, suggesting underlying APD.
Initial assessment and findings
Jackie’s initial audiogram showed hearing thresholds within normal limits, and speech audiometry results were near perfect. A Quick Speech in Noise (Quick SIN) screening test revealed results within normal limits. However, using the HHIA, Jackie scored 82 out of 100, indicating a severe impact of hearing difficulties on her psychosocial wellbeing [2]. This stark difference between her audiometric test results and HHIA score suggested that her challenges were unrelated to hearing sensitivity but possibly due to auditory processing difficulties.
"The goal is not to label the individual with a diagnosis, but rather to pinpoint specific areas of auditory skill weakness that can be addressed with targeted interventions."
Auditory processing evaluation
A comprehensive APD evaluation was conducted using the Buffalo Model Central Test Battery (CTB) to further explore Jackie’s condition. This assessment included the Speech in Noise (SIN) test, Staggered Spondaic Words (SSW) test, and Phonemic Synthesis (PS) test [3]. These tests evaluate different aspects of auditory processing, such as the ability to understand speech in noisy environments, dichotic listening (processing different sounds presented to each ear simultaneously), and phonemic awareness (recognising and manipulating speech sounds). Jackie’s performance on these tests confirmed difficulties consistent with APD.
Intervention: auditory training
Given the severity of her auditory processing difficulties, Jackie was enrolled in a 12-week auditory training programme based on the Buffalo Model. This training included exercises to improve phonemic awareness, speech understanding in noise and short-term auditory memory.
Therapy outcomes
Over the course of the therapy, Jackie showed marked improvements. Her HHIA score dropped from 82 to 24, indicating a significant reduction in the perceived impact of her hearing difficulties on daily life. Follow-up assessments continued to show improvements, and Jackie reported enhanced self-esteem, less fatigue and a newfound enjoyment of music and television.
A comprehensive APD re-evaluation demonstrated auditory processing test results that were within normal limits bilaterally. At a two-year follow-up without any additional interventions, Jackie was asked if she senses that she still has APD, to which she responded, “That’s a good question… No.” Her progress, demonstrated by her HHIA scores, is presented in Figure 1.
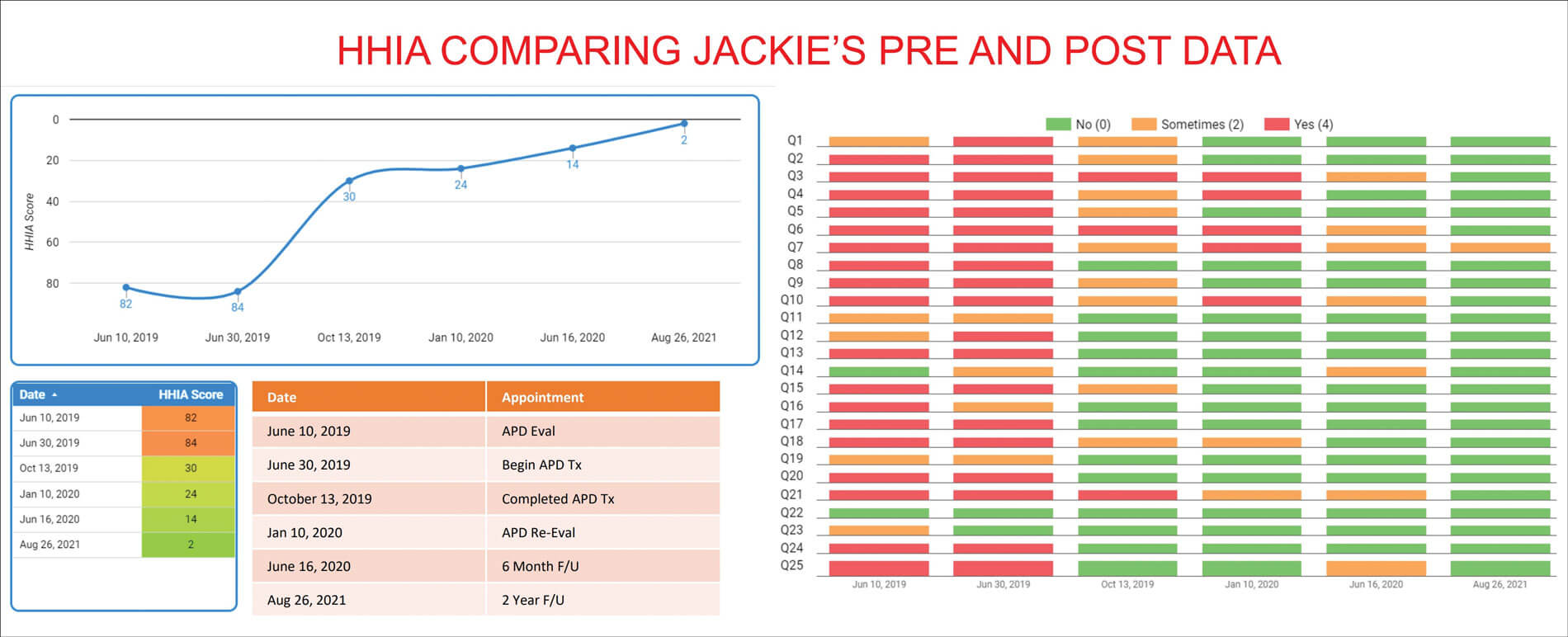
Figure 1: Jackie’s HHIA progress results throughout auditory training.
The role of the HHIA in clinical practice
Jackie’s case highlights the utility of the HHIA as a diagnostic and outcome measure in clinical practice. By incorporating the HHIA into routine evaluations, audiologists can:
- Identify APD red flags: The HHIA helps to recognise potential auditory processing issues in individuals with normal audiometric findings, guiding further testing and interventions.
- Track progress: Repeated HHIA assessments can monitor the effectiveness of treatment, such as auditory training and / or the use of low-gain devices.
- Enhance client-centred care: Engaging clients with the HHIA can provide valuable insights into their experiences and challenges, allowing for tailored intervention strategies.
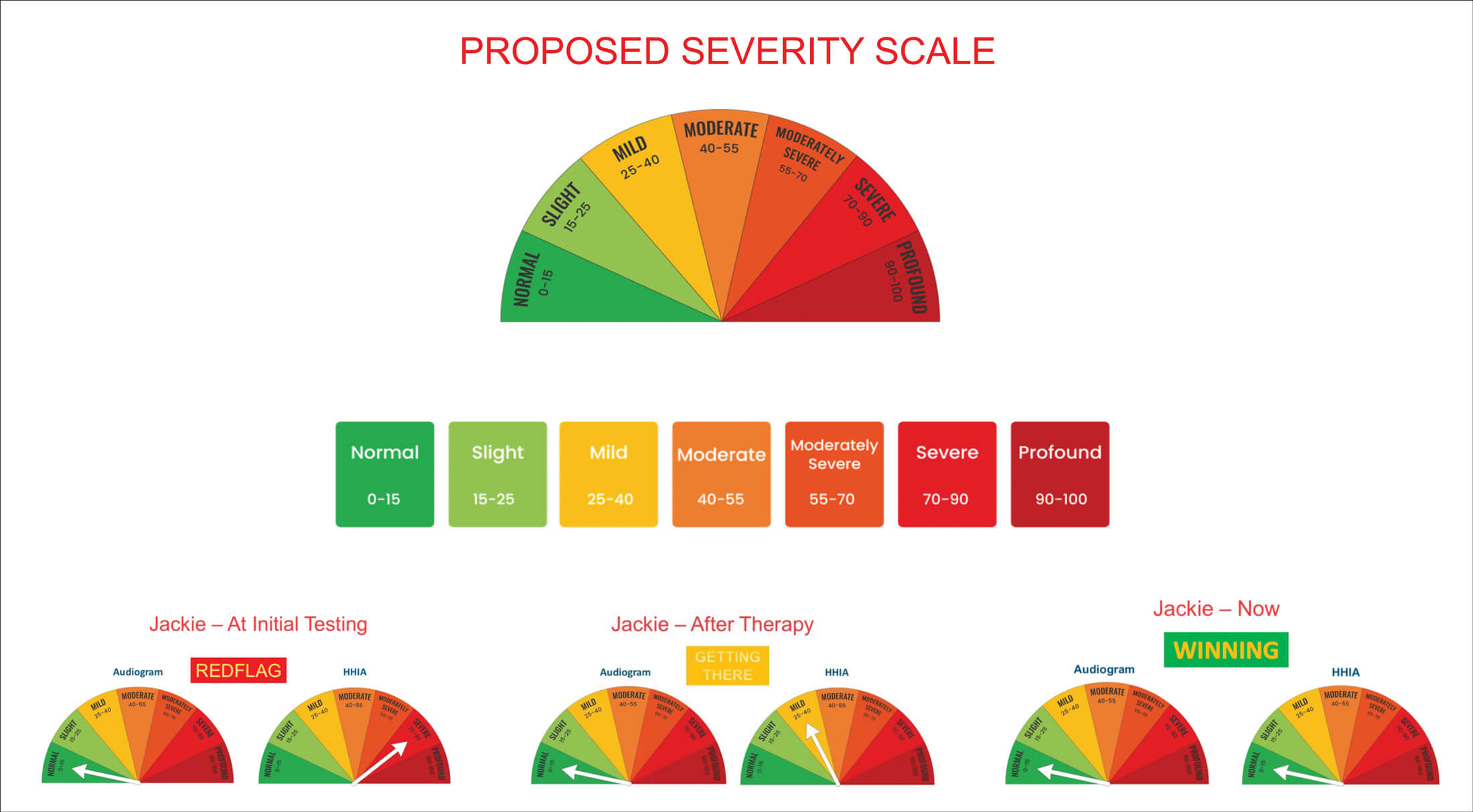
Studies question the validity of HHIA due to its weak correlation with audiograms, especially speech scores [1]. This mismatch, however, can be a strength in detecting red flags for auditory processing difficulties when audiometric results are normal. We propose a severity scale to compare HHIA scores to audiograms. A mismatch may indicate APD, warranting further evaluation. The goal is to achieve the lowest HHIA score regardless of hearing sensitivity. The current HHIA severity range is too broad, hindering accurate severity distinction. A more nuanced scale, suggested in Figure 2, would allow for better comparison with audiograms.
Recommendations for clinicians
To effectively use the HHIA in identifying and managing APD, clinicians should consider the following steps:
- Screening: Administer the HHIA to all clients reporting hearing difficulties, regardless of audiometric results. High scores may indicate the need for further investigation and potential APD evaluation.
- Intervention: For individuals with high HHIA scores and normal audiograms, consider an APD evaluation, followed by auditory training and / or fitting low-gain devices.
- Monitoring: Use the HHIA regularly to track progress and adjust interventions as needed. Improvements in HHIA scores can indicate successful management of hearing difficulties.
Practical application: fitting low-gain devices
A recent study demonstrated the benefits of using low-gain hearing aids for individuals with normal audiograms but high HHIA scores. The study found that those with HHIA scores above 34 perceived significant benefits from low-gain amplification [4]. Based on these findings, clinicians could use a cookbook approach similar to the one suggested below:
- Pre-fitting assessment: Administer the HHIA and conduct a comprehensive hearing assessment. Note any discrepancies by comparing the audiometric results to those of the HHIA, as previously illustrated using the suggested severity scale in Figure 2.
- Device fitting: If a mismatch is found, proceed to fit low-gain hearing aids. Hearing aids settings can be guided by the study mentioned above, with an insertion gain of 5–10 dB for soft / conversational inputs between the 1000–4000 Hz frequency range. Louder sounds are not provided any amplification [4].
- Follow-up: At the follow-up appointment, reassess using the HHIA to determine if scores have significantly dropped, indicating effective intervention. Repeat the reassessment on a regular basis to make sure the patient still perceives continuous benefits from their devices.
- Adjustments: If there is no improvement in HHIA score, at least at the first stages of intervention, additional considerations need to be made. Consider adjusting hearing aid programming settings, trialling a different brand of hearing device or a trial of a remote microphone device.
- Further referral: Persistent high scores despite intervention may warrant referral to an auditory processing specialist for further intervention. This typically includes a comprehensive APD evaluation, after which auditory training in addition to the low-gain amplification would be planned accordingly.
Addressing auditory processing difficulties in people with hearing loss
While hearing aids are crucial in addressing hearing loss, it is essential to recognise that these devices may not fully resolve all of the communication difficulties individuals experience. Individuals with hearing loss have a higher likelihood of experiencing challenges in processing the sounds secondary to their hearing loss. For example, we might suggest a proactive approach similar to that of the client with a normal audiogram: check their HHIA score before fitting with amplification and use a follow-up HHIA post-trial to see how their scores may change. If their HHIA does not improve significantly post-hearing aid trial, additional specialist testing and auditory training may be recommended. The goal is not to label the individual with a diagnosis, but rather to pinpoint specific areas of auditory skill weaknesses that can be addressed with targeted interventions. Once again, the HHIA can be used to monitor the effects of the intervention.
While access to auditory processing services for individuals with hearing loss is still evolving, the growing availability of such specialised clinics represents a positive step towards providing more comprehensive and effective care for this population.
Discussion
Please note that Jackie received auditory training instead of low-gain devices. However, in a similar discussion, we raised the question: ‘What if we had fit Jackie with low-gain hearing aids and not offered auditory training?’
- Would she still be wearing them?
- Would she still feel like she has APD?
- Would she need to worry about moisture / wax and charging them every night?
- Would she have a remote microphone?
- How much would she have paid for this technology?
- How often would she need to replace the hearing aids?
- Would this have been in her best interest? [5]
Conclusion
The HHIA is a valuable tool for identifying and monitoring potential APD red flags, particularly in adults who report hearing difficulties despite a normal audiogram. By incorporating the HHIA into clinical practice, audiologists can better identify clients who might benefit from low-gain devices and auditory training. Jackie’s case demonstrates that significant improvements in quality of life are possible with the right intervention. This approach not only addresses auditory challenges but also enhances overall wellbeing, ensuring clients live life more fully.
"By incorporating the HHIA into clinical practice, audiologists can better identify clients who might benefit from low-gain devices and auditory training."
By leveraging tools like the HHIA, clinicians can adopt a more holistic approach to hearing care, addressing both the physiological and psychosocial aspects of auditory processing disorders. This, in turn, leads to better patient outcomes and higher satisfaction, marking a significant step forward in the field of audiology.
Next steps
You are invited to watch a 20-minute lecture to learn more about using the HHIA and integrating it into your clinical practice.
Click here for a free copy of the HHIA for your clinic and a video featuring Jackie’s firsthand experience with APD and her journey to better and sustained outcomes.
References
1. Newman CW, Weinstein BE, Jacobson GP, et al. The hearing handicap inventory for adults: psychometric adequacy and audiometric correlates. Ear Hear 1990;11(6):430–33.
2. Newman CW, Jacobson GP, Hug GA, et al. Perceived hearing handicap of patients with unilateral or mild hearing loss. Ann Otol Rhinol Laryngol 1997;106(3):210-4.
3. Katz J. APD evaluation to therapy: the Buffalo Model. Audiology Online 2007.
https://www.audiologyonline.com/articles/
apd-evaluation-to-therapy-buffalo-945
[Link last accessed December 2024].
4. Roup CM, Post E, Lewis J. Mild-gain hearing aids as a treatment for adults with self-reported hearing difficulties. J Am Acad Audiol 2018;29(6):477–94.
5. Alexander A and Abbas F. How to Spot an Adult with Auditory Processing Disorder. ACCORD September 2024.
Declaration of competing interests: AA owns and operates the Auditory Processing Institute (API) which offers paid online courses on auditory processing testing and auditory training.










