COVID-19 has ravaged the world in the past 18 months. The second wave in many countries was deadlier than the first. Mucormycosis, infamously labelled ‘the black fungus’ has affected some countries, such as India, in epidemic proportions within this COVID pandemic. Dr Sunil Narayan Dutt, Global Ambassador for ENT & Audiology News, interviews two expert surgeons, Dr Deepak Haldipur and Dr Aditya Moorthy, who have worked tirelessly in trying to save the lives of patients with mucormycosis in the city of Bangalore, India.

Dr Deepak Haldipur and Dr Aditya Moorthy.
Welcome Dr Deepak Haldipur and Dr Aditya Moorthy. As a team, you have looked after more than 300 patients with rhino-orbito-cerebral mucormycosis (ROCM) and COVID-associated mucormycosis (CAM) in Bangalore. What, according to you, have been the most significant predisposing factors for CAM, particularly in India?
We have had a bit of experience last year with a spurt of mucormycosis in the first wave of COVID. Our publication last year raised the spectre of an epidemic within the pandemic with a combination of diabetes mellitus (uncontrolled), steroids (indiscriminate use) and the Sars-CoV 2 setting up an ‘unholy trinity’ (a term that caught on in the Indian media) of predisposing factors. This time around, the Delta variant of the disease has proven to be far more devastating. In spite of the wide tabloid speculation, these three seem to be the strongest correlative factors for mucor.
What is the clinical course of ROCM in relation to COVID on its timeline?
While a few mucor infections were seen between the seventh and 14th day of COVID illness (5% or less), the majority were seen between day 14 and day 45. Very few (less than 5%) had commencement of mucor symptoms after day 45. These numbers are a rough estimate as we still are in the midst of the mucor epidemic.
What advice would you give our colleagues treating COVID (GPs, physicians, intensivists) in terms of preventive measures for ROCM/CAM development?
Cautious use of corticosteroids, strict glycaemic control and a high index of suspicion in considering mucor as a diagnosis are vital. Liberal use of diagnostic nasal (video) endoscopy (DNE) in high-risk groups (post-COVID status, poorly controlled diabetics and extensive use of steroids) is strongly recommended.
“Any patient who presents with facial pain (mostly unilateral), paraesthesia (generally over the malar region), unilateral nasal block and mobility of teeth on the same side would be a ‘mucor suspect’”
So would you recommend nasal endoscopy/KOH mount/CT scan sinuses for all patients with moderate to severe COVID admitted to hospital?
Shotgun investigations would be an overkill, especially imaging. Nasal endoscopy would be useful in high-risk patients, most definitely.
Who is a ‘mucor suspect’?
Any patient who presents with facial pain (mostly unilateral), paraesthesia (generally over the malar region), unilateral nasal block and mobility of teeth on the same side would be a ‘mucor suspect’. Other obvious presentations include eye pain, ptosis, proptosis, ophthalmoplegia and discolouration over facial skin.
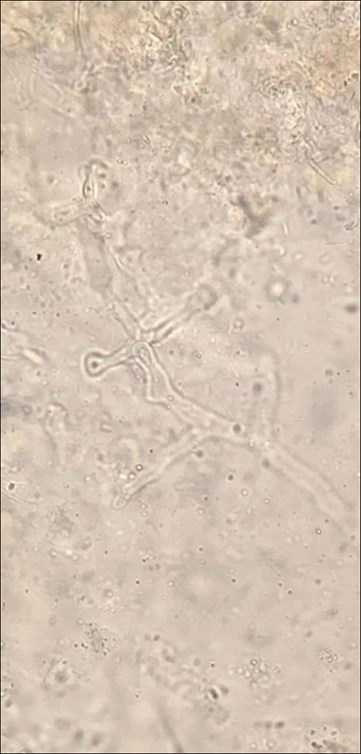
KOH slide depicting the fungus.

Endoscopic view of pus drained from a frontal lobe abscess through the cribriform plate.
What investigations would you perform on such a suspect and in what order?
ENT/oral/neurological/ophthalmic examinations, video nasal endoscopy, KOH mount of tissue plug (not swab), MRI brain with orbit and PNS with contrast (fat suppressed) (with a Screening CT of PNS and face) are performed. An exhaustive but practical scoring/staging system is available from radiology that we use. The definitive specimens can be sent for special fungal stains (PAS, GMS), fungal culture and histopathological examination.
“Surgical management may range from orbital decompression to selective periorbital endoscopic debridement to orbital exenteration (guided by clinical and radiological findings). Most decisions are tailored to the context”
Please enumerate all the specialists involved in your multidisciplinary team for managing ROCM.
ENT/rhinologist/skull-base surgeon, maxillofacial surgeon, ophthalmologist/oculoplastic surgeon, neurosurgeon, infectious diseases specialist, intensivist, anaesthesiologist, physician, neurologist, nephrologist, radiologist, microbiologist/mycologist, pathologist, psychiatrist and dietician. Each specialist would be enrolled as required at different stages.
How exhaustive is your consent form? Is it important to take a video consent? Could you share a copy of your consent form?
Exhaustive counselling is as important as a detailed consent. Video consent is very useful in the medicolegal context and needs to be done in the language the patient and caregivers speak. The consent form prepared by the Association of Otolaryngologists of India (AOI) is being used now and we are happy to share the same on email upon request.


MRI scans of a patient with ROCM showing a large frontal lobe brain abscess
with necrosis of the cribriform plate (coronal and sagittal views).
No one would contest the fact that ‘adequate surgical debridement’ of the diseased tissues must be performed on an emergency basis. How do you decide your debridement is ‘optimal’?
In advanced presentations, especially with retro-orbital, retromaxillary disease with loss of vision, irreverent excision of diseased and devitalised tissues with a low threshold for orbital exenteration may have to be considered. In indolent disease, we aim for ‘bleeding healthy (pink) tissue and bone/marrow’ with a reasonable attempt at conservation (anatomical and functional).
What percentage of patients in your series is with ‘orbital disease’ and with ‘intracranial disease’? How have you managed them?
The initial phase saw late presentations including cerebral mucormycosis. But overall, cerebral involvement is about 5-8%. Also, 2-3% of other patients progress to intracranial involvement in spite of aggressive treatment. Cerebritis is managed conservatively with significantly higher doses of amphotericin B. Focal abscesses have been drained by neurosurgeons. About 20% of patients have had some degree of orbital involvement. Surgical management may range from orbital decompression to selective periorbital endoscopic debridement to orbital exenteration (guided by clinical and radiological findings). Most decisions are tailored to the context.
“It is hard to speculate but there is the possibility of a third wave should we drop our guard and not learn lessons from the first and second waves”
Share your thoughts on amphotericin B treatment. How is the scarcity of the medication being addressed in India? Do you believe this is detrimental to the outcomes?
When left with no choice, doctors may be forced to triage the amphotericin available (liposomal or conventional) for worse disease (orbital, skull base, intracranial) and use second line antifungals for those diseases with possibly better prognosis (sinonasal disease). Inadequate amphotericin dosage is certainly detrimental to the outcome. Close monitoring of renal and liver function is essential with antifungal treatment.

Endoscopic picture of mucor with necrotic tissue in middle meatus.

The operating team in action.
Do you recommend use of local forms of drug delivery (topical, irrigations, infiltrations-injections)?
Local drug delivery has been attempted in the forms of packs coated with amphotericin gel. Some believe in using ampho irrigations for the cavity. The use of TRAMB, retro-orbital injections of ampho-B, has also been widely discussed. However, there is lack of evidence these treatments work. Time will tell.
What is your postoperative monitoring protocol with the surgically created cavity?
We perform pack removal after 48 hours with meticulous endoscopic cleaning/toilet/debridement on the seventh, 17th and 27th day. All maxillectomies and open maxillary explorations are packed with BIPP (bismuth iodoform paraffin paste) that is changed after five to seven, days and removed in two weeks. The pack change/removal coincides with the planned surveillance scans, MRI with contrast. Scans are usually at weekly intervals unless dictated otherwise.
Could you talk a bit about ‘drug holidays’ and ‘combination therapies’?
Drug holidays are mostly enforced by other factors, such as unfavourable renal parameters, erratic supply of amphotericin B or drug reactions. Combination therapies have little scientific basis but for the two or three days of overlap, when amphotericin therapy is switched to (step-down) posaconazole or isavuconazole for maintenance.
“While the term ‘black fungus’ is inaccurate, it struck a chord and ingrained itself in the public psyche. This certainly resulted in them seeking help early and early referrals from GPs”
What approximately is the total duration of treatment? When do you decide and hence declare a patient with ROCM/CAM as ‘cured’ of disease?
Liposomal amphotericin B is administered to a cumulative dose ranging from 5-10gms (depending on the severity/staging of the disease). The dosage varies from 3-5mg/kg/day to 10mg/kg/day for a total of 10 to 20 days (two to three weeks). If it is the conventional (deoxycholate) Amphotericin, it is usually for 21 to 42 days (three to six weeks) depending on the extent/severity of the disease. This is followed by oral posaconazole or isavuconazole for a total of 12 weeks (three months). The patient is deemed ‘cured’ if he/she remains clinically and radiologically disease free after this period. We generally look forward to the 100th day for ‘cure of disease’.
Is there a role for ‘stand-alone’ antifungals, i.e., without surgery in post-COVID mucor?
Probably yes, in advanced inoperable cases, cases postponed due to poor lung/general conditions, and in those that refuse the surgery as a treatment modality.
Briefly tell us about the disfigurements that these patients may sustain and your rehabilitation plans for the same.
Two of the most devastating and lasting disfigurements are loss of the globe and loss of the maxilla with its associated teeth leading to severe functional, social and emotional debilitation. Immediate/intermediate feeding plates and prostheses are provided temporarily followed by more elaborate obturators that can be tissue or implant supported.
What is the mortality related to this disease in your series and in the country, in general?
Mortality is around 20% (both with us and in the country) and usually with extensive intracerebral disease. Some others die of COVID-related pulmonary/cardiac/renal complications (multi-organ failure).
The second wave (Delta variant) has really hit us hard and the mucor epidemic has paralleled the COVID pandemic wave. Delta Plus is now a variant of interest and concern, and there is talk of a third wave supported by many experts and epidemiologists. Will there be another mucor epidemic?
It is hard to speculate but there is the possibility of a third wave should we drop our guard and not learn lessons from the first and second waves. And, should there be a third wave, another mucor surge may be inevitable.
There is the fear of the ‘black fungus’ (and white fungus and yellow fungus) amongst the public: ‘mucor phobia’, some call it. How do we allay this fear and reassure them?
Indeed. But for once, the media have played a positive role in early pick up and treatment and mostly rational relay of information. While the term ‘black fungus’ is inaccurate, it struck a chord and ingrained itself in the public psyche. This certainly resulted in them seeking help early and early referrals from GPs.
List some Dos and Don’ts specifically in relation to fungal infections for the general public.
- Wear a mask
- Social distance
- Hand wash/sanitise
- Restrict social gatherings
- COVID-appropriate behaviour
- Strict glycaemic control
- Cautious use of steroids
- No self-medication
- Early specialist consultation in a mucor suspect
I have heard colleagues (and I concur with them) describe this as a ‘dehumanising disease’. How have you and your teams coped with COVID and this fungal epidemic emotionally?
The sheer magnitude of the disease has cast the doctor in the role of a God Player, with the resultant emotional and psychological stress leaving some shell-shocked (some even needing psychological help). It is vital to maintain positivity and perhaps even a certain degree of detachment to maintain order in all this chaos. So, “don’t try to play God; you can only do your ‘karma’; if you become an emotional cripple, who will do your job?; focus on what you can salvage rather than what is lost; only a smiling and positive care provider can help a patient, not a sulking one,” are some of the oft-repeated quotes.






